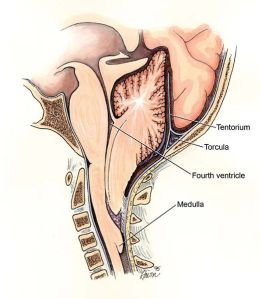
 Chiari malformations are typically associated with herniation of the brainstem into the foramen magnum in the base of the skull as shown in the picture on the left. More recently, it has come to include what is called a Zero Chiari Malformation in which the cerebellum comes in contact with the base of the cranial vault without herniation into the foramen magnum. This has prompted some researchers to suggest that Chiari malformations include any decrease in cerebrospinal fluid volume (CSF) sufficient enough to cause the brain to sink and come in contact with the bones of the base of the skull.
Chiari malformations are typically associated with herniation of the brainstem into the foramen magnum in the base of the skull as shown in the picture on the left. More recently, it has come to include what is called a Zero Chiari Malformation in which the cerebellum comes in contact with the base of the cranial vault without herniation into the foramen magnum. This has prompted some researchers to suggest that Chiari malformations include any decrease in cerebrospinal fluid volume (CSF) sufficient enough to cause the brain to sink and come in contact with the bones of the base of the skull.
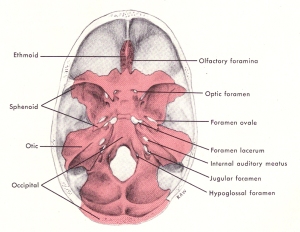 Considering the above, in addition to the foramen magnum there are other large holes in the base of the skull through which cranial nerves and blood vessels pass, as seen in the picture on the right. It is possible that the cranial nerves may herniate into the openings or come in contact with the base of the skull due to Chiari malformations in which the volume of CSF falls too low, as mentioned above. The consequence would be similar, as well, that is cause compression of nerves and circulatory routes.
Considering the above, in addition to the foramen magnum there are other large holes in the base of the skull through which cranial nerves and blood vessels pass, as seen in the picture on the right. It is possible that the cranial nerves may herniate into the openings or come in contact with the base of the skull due to Chiari malformations in which the volume of CSF falls too low, as mentioned above. The consequence would be similar, as well, that is cause compression of nerves and circulatory routes.
 The brain floats within the cranial vault. Typically, it is prevented from sinking into the foramen magnum by the cisterns of the brain which are filled with cerebrospinal fluid (CSF). The cisterns are also strategically placed to provide cushioning, support and protection from the hard bones of the cranial vault as seen in the picture on the left.
The brain floats within the cranial vault. Typically, it is prevented from sinking into the foramen magnum by the cisterns of the brain which are filled with cerebrospinal fluid (CSF). The cisterns are also strategically placed to provide cushioning, support and protection from the hard bones of the cranial vault as seen in the picture on the left.
Symptoms of MS often include cranial nerves. Common complaints include dizziness, ringing in the ears or loss of hearing, trigeminal neuralgia, burning tongue and dry mouth. By far, however, the cranial nerve most commonly involved in MS is the optic nerve. Optic neuritis is, in fact, one of the most frequent symptoms of MS. Even Asians and African-Americans who, otherwise, have a much lower incidence of MS, get optic neuritis. They also get transverse myelitis, but that’s another topic entirely. I will be covering the different cranial nerve signs, as well as transverse myelitis on my new website starting with the optic nerve.
The optic nerve is the second most superior (highest) nerve in the cranial vault. The highest cranial nerve is the olfactory nerve to the nose which is located in the anterior fossa or forehead area of the base of the skull. The optic nerve lies in the middle fossa behind the eye sockets. Most of the cranial nerves are in the posterior fossa along with the brainstem and cerebellum.
It’s position in the cranial vault and the optic canal may be the reason why optic neuritis is one of the most common signs and symptoms of MS, optic-spinal MS and Devic’s disease. Typically, the optic nerve is protected by the chiasmatic cistern, which is one of the highest cisterns in the brain. Among other things trauma and failure of the CSF support system of the brain may play a role in optic neuritis. For further information on optic neuritis click on the link below to my new website. The website can also be found in the links section of the sidebar under upright-health.

I know a young girl who has Dystonia. I can see links here with Ms. Does Dystonia connect any dots with your amazing work.. It is known as a primary condition.. utmost regards.
Hello Sheridan, Dystonia is a different topic but it does share certian similar characteristics related to my research. In particular, it appears to affect the basal ganglia of the brain similar to Parkinson’s disases.
Help! I will try to keep this short and sweet. At age 14 my daughter was in an automobile accident suffering from neck & back pain, and severe daily headaches. (she was twisted at the waist, turning to talk to the girl behind her when the car was struck) From that night forward she has not been the same. Ten years later we finally got an MRI because her pupils were uneven. The MRI revealed Chari I Malformation. Nothing was done until they finally, a year later, discovered a lesion/syrinx on her spinal column which indicated restricted CSF. She finally had decompression surgery in October 2010. But, In addition to the uneven pupils and the symptoms described above. She has had many strange symptoms that doctors say are not related………falling down at times, difficulty swallowing or chocking, severe stomach pains, irregular menstrual cycles, cold hands & feet with discoloration, tingling and numbness. (diagnosed with reynauds last week) Recently, all of her hormones tested below the levels of a menopausal women. (appear to be normal now) Her thyroid was supposedly not functioning. Prescribed medication by one doctor only to be taken off by another. My question to you; Is there any correlation between any of these symptoms? We had our last visit with the neuro-surgeon yesterday. The syrinx in the upper spine appears to be gone according to the latest MRI. However, they have never looked at her entire spine. Could there be something going on that they’ve missed? Something that could explain some of these other symptoms? I should also reveal that her grandfather (on her father’s side) had Parkinson’s and a cousin has MS.
Worried Mom!
While I can’t speak for all of your daughter’s “strange symptoms” I can tell you without doubt that some of the symptoms she is/was experiencing is related to the CM1 diagnosis. I know this without doubt because I too have CM1 for which I underwent surgery. I had many of the same symptoms as your daughter; the falling down, difficulty swallowing/choking, tingling/numbness. During the long, drawn out process of finding the correct diagnosis for my symptoms, I also was tested for thyroid problems. My symptoms also started as the result of related trauma but research states that many people probably have the CM1 condition but until a trauma of some type happens, the condition does not affect the person. Given that only approximately 3% of the US population is ever truly diagnosed with CM1, it is commonly overlooked or mis-diagnosed. Luckily I was blessed with a fabulous neurosurgeon who didn’t “jump the gun” and diagnose me with MS which is so often the case. I do however find it interesting that you have a family history of MS. This is interesting to me because years after my diagnosis of CM1, my brother was diagnosed with MS. His neurologist assures us that CM1 was ruled out as a possibility for his symptoms but since him and I are the only 2 people in our entire family (that anyone can remember) with any neurological conditions, we are convinced that MS and CM1 must somehow be related.
If your daughter has presistant symptoms, I would re-visit the neurosurgeon or get a 2nd opinion. Research also shows that some patients require additional surgeries/decompression.