The root of the word sclerosis means scar and multiple sclerosis is associated with multiple scars in the brain. Scars being what they are, it is unlikely that either the best upper cervical chiropractic care or surgical liberation procedure will lead to repair of badly damaged or scarred tissues.
If you read the comments section you will see that many people with MS lesions recall severe trauma from many years earlier. Only in rare cases do the serious symptoms show up immediately or soon after trauma so no one would even think of looking for lesions in the first year or so after the accident. In fact, the interval of time between the traumatic incident and the onset of symptoms and lesions is one of the key issues in the medicolegal debate regarding the relationship between MS and trauma. The other issue is the cause or mechanism of injury. I discuss the medicolegal issue, as well as a pertinent clear cut case or MS related to whiplash in my book.
By the time brain scans are done the scars can be many years old. On the other hand, I had the experience of treating cases where the signs, symptoms and lesions all started to show up in just about a year. Two of those cases were especially severe and resulted in significant disabilities. In any case, most lesions in MS are permanent scars.
Unfortunately, oftentimes the scars are in bad locations as far as signs and symptoms are concerned. For example, the cervical cord contains all of the long myelinated tracts that pass from higher centers in the brain down to the arms and legs to work the muscles. Damage to these long tracts can cause permanent muscle weakness. The goal in these cases should be to restore function and halt further progression and disability as much as possible.
The lesions or scars of multiple sclerosis show up as bright spots called hyperintensity signals on MRI as seen in the brain scan on the right. Hyperintensity signals, however, are not unique to MS. Strokes and migraine headaches can also cause hyperintensity signals on brain scans in the area of impaired arterial blood flow.
called hyperintensity signals on MRI as seen in the brain scan on the right. Hyperintensity signals, however, are not unique to MS. Strokes and migraine headaches can also cause hyperintensity signals on brain scans in the area of impaired arterial blood flow.
MS hyperintensity signals are more characteristically located above the covering over the posterior fossa, which contains the cerebellum as seen in the sketch below. Hence, the covering is called the tentorium cerebelli. MS lesions are typically found in supratentorial areas. Additionally, the hyperintensity signals are often found surrounding the chambers in the core of the brain called ventricles in the periventricular areas. The ventricles are the dark shadows in the brain scan above and chambers in the middle of the brain and brainstem seen in the sketch below.
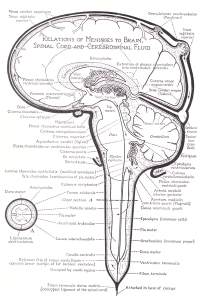 In addition to the supratentorial and periventricular areas, instead of arteries, as in strokes and migraine headaches, the lesions in MS are more typically found in what are called perivenular areas around the larger dural sinuses (veins) of the brain. They also tend to get smaller in number and size as you follow the blood vessels upstream counter-current to blood flow. This is the complete opposite of what you would expect if viruses were the cause because viruses follow blood flow. Consequently, the lesions would tend to show up in areas closer to the source of the stream in the arteries first, not so much further downstream in veins. Considering all the above, it’s hard to picture how stenosis in such distant jugular and thoracic veins could cause lesions to show up predominantly in the higher and core areas of the brain above the tentorium, and not more in the cerebellum, which is down in the basement of the cranial vault called the posterior fossa.
In addition to the supratentorial and periventricular areas, instead of arteries, as in strokes and migraine headaches, the lesions in MS are more typically found in what are called perivenular areas around the larger dural sinuses (veins) of the brain. They also tend to get smaller in number and size as you follow the blood vessels upstream counter-current to blood flow. This is the complete opposite of what you would expect if viruses were the cause because viruses follow blood flow. Consequently, the lesions would tend to show up in areas closer to the source of the stream in the arteries first, not so much further downstream in veins. Considering all the above, it’s hard to picture how stenosis in such distant jugular and thoracic veins could cause lesions to show up predominantly in the higher and core areas of the brain above the tentorium, and not more in the cerebellum, which is down in the basement of the cranial vault called the posterior fossa.
In addition to the brain, MS lesions are sometimes found in the cervical cord as depicted in the old sketch above. In contrast to the core of the brain, lesions in the cord tend to show up on the outside along its flanks which contain the myelinated tracts mentioned above. Rarely ever do MS lesions show up below the shoulders. While MS lesions stop at the shoulders, however, other similar conditions associated with scarring similar to demyelination seen in the cervical cord in MS, are seen in the lower cord, such as amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease and primary lateral sclerosis (PLS). A variant of ALS, PLS can reach up into the brain as well. It’s called bulbar ALS. There is also a variant of MS, called Devic’s disease, that is associated with demyelination in the lower cord but optic neuritis in the brain. In addition to MS, I also treated patients with demyelinating diseases of the lower cord. At this time there is nothing anyone can do to stop the devastation in these conditions, but I believe we are getting closer, and a flood of cranked-up highly motivated MS patients are leading the way. When Parkinson’s patients join the fray the pressure will increase three fold, so will the money for further research into venous drainage problems.
Interestingly, while Asians have a lower incidence of MS they do get demyelinating diseases of the cord such as Devic’s disease. I believe it has to do with design differences between Caucasian and Asian skull designs. I will be covering demyelinating diseases of the lower cord on my new website, which is not quite ready for public viewing yet. Suffice it to say that demyelinating diseases of the cord are probably due to similar design problems and circulatory causes found in MS.
As far as the cause and location of the lesions of MS are concerned, Dr. Schelling’s theory makes the most sense. I will be discussing Schelling’s theory as to why the lesions show up where they do in my next post. I will also throw in some of my own two cents to add to the mix and maybe fill in some of the gaps. In brief, I believe that in certain cases of MS the hyperintensity signals and lesions are more likely due to decreased arterial blood flow similar to migraines and mini strokes, not venous drainage problems.
While curing the scars may be difficult or impossible, the location of the scars are often in areas that have nothing to do with many of the unusual signs and symptoms associated with MS, such as optic neuritis, ringing in the ears, trigeminal neuralgia, speech problems, balance problems, fatigue etc. Even more interesting is that, except for the eyes, most of the nerves that would cause such symptoms are found below the tentorium in the posterior fossa. Most of the signs and symptoms associated with Parkinson’s disease likewise come from the posterior fossa. Slowly but surely, trauma is being recognized as a possible causative factor of Parkinson’s just like MS. Furthermore, since the lesions don’t come and go in MS they can’t be the cause of remissions and exacerbations of signs and symptoms. This is a promising fact!
Halting the progression of MS and improving signs and symptoms unrelated to the lesions is definitely possible by restoring fluid mechanics in the brain. Upper cervical correction is one way to do it. The liberation procedure is another. We are on a completely new path but we have only taken the first step. Things can only get better as we learn more and continue to unravel the mystery of MS and the unique design of the incredible human brain due to upright posture. I believe upright MR and angiograms will shed much more light.


I have had PLS for at least 25 years. It is generally recognized as an upper motor neuron disease, not a demyelinating disorder. Neither is ALS a demyelinating disease and it differs from PLS because it involves the death of both upper and lower motor neurons. ALS is life threatening; PLS is not.
Thanks for your comment. ALS and PLS are categorized as MN diseases. UMN diseases interfere with the primary neuron pathways between the brain and spinal cord. Both conditions, however, are associated with scarring of myelin tracts in the cord similar to the scarring in the cervical cord seen in MS, which is attributed to demyelination. Technically, MS isn’t categorized as a demyelinating disease either. It’s typically categorized as an autoimmune disease even though there is little evidence to support such claims. Some cases of MS show no signs of scarring but they do have UMN signs. What’s more, MS patients have lesions higher up in the brain that can affect UMN pathways. ALS for example tends to affect motor neurons of cranial nerves and cerebellum lower down in the brainstem not high up in the motor cortex. Lastly, myelin may not be the first thing to breakdown in MS. The neuron inside may actually precede it. Demyelination has also been show in Alzheimer’s and Parkinson’s patients as well. It is probably part of a more general degenerative process. Interestingly, Parkinson’s disease affects UMN type pathways in the brain that modify primary motor neuron signals coming from the motor cortex. In my opinion, all these conditions should all be categorized as neurodegenerative diseases.
I was referring to the more fatal nature of ALS cases. On the other hand, Stephen Hawkins has survived with ALS for decades.
hi!This was a really magnificentsuper post!
I come from usa, I was fortunate to search your subject in wordpress
Also I get much in your topic really thanks very much i will come again
Thanks. Glad you enjoy it. I am flattered that you understand it as that is my goal.
Hello, thank you for this! As much as there is quite a bit that I do not understand (my studies are nowhere near anything scientific, besides environmental), I found this really interesting and I will delve deeper into your website. It is great to see that you are taking the time to put out your research for people like me who have MS and want to learn and then do something about it!
Thanks 🙂
Oh my goodness, who IS this person?! This is the most intelligently written science-medico article I have ever read in my life! (and I do read a bit; enjoy a subscription to Science magazine, where some of the articles are inpenetrable). I have a brother-in-law, very well-respected heart surgeon, whose wife has MS (she is a GP). We have no idea what MIGHT cause this. Amazing.
Hello Estie,
Thanks for the compliment. Have your brother-in-law or his wife contact me. Perhaps we can get to the bottom of what caused the condition.