According to Schelling venous back jets into the brain and shear stresses in the cord combined with cerebrospinal fluid reflux are likely causes of demyelination. Other researchers have suggested that chronic edema and normal pressure hydrocephalus can damage myelin simply by stretching it. Zamboni suggests that venous drainage problems lead to iron accumulation, which initiates neurodegenerative processes. There is still another theory that suggests that demyelination may be due to chronic ischemia, that is, decreased blood flow to the brain and cord. For now, I will focus on the blood supply to the brain and ignore the cord.
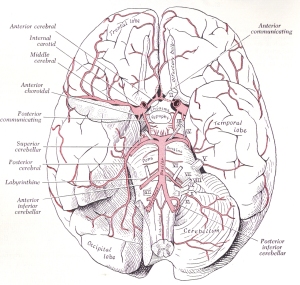
As depicted in the picture above, blood is delivered to the brain via the anterior and posterior blood supply routes. The anterior blood supply routes are the internal carotid arteries. They are called anterior because they are in the front of the neck. The posterior blood supply routes are the vertebral-basilar arteries in the back of the neck. The carotid arteries travel along either side of the trachea (windpipe) and enter the brain through an opening in the base of the skull called the foramen lacerum where it passes through the cavernous sinus of the drainage system of the brain. (Click on any picture to enlarge it and get a closer view).
As shown in the picture above, the vertebral arteries pass through holes in the transverse processes of the cervical spine. They exit the spine at the first cervical vertebra and enter into a memebrane between the base of the skull and the first cervical vertebra. The membrane is called the suboccipital cavernous sinus or atlantooccipital membrane as seen in the picture on the right.
After traveling through the suboccipital cavernous sinus for a short distance the vertebral arteries turn in and head upward. They next pass through the foramen magnum as shown in the picture on the left. Shortly after passing through the foramen magnum the vertebal arteries unite to become the basilar artery. Before uniting the vertebral artery gives off two branches. One is called the posterior inferior cerebellar artery because it supplies the lower rear aspect of the cerebellum. The other artery is called the anterior spinal artery.
The two anterior spinal arteries then unite and head back down through the foramen magnum to supply the entire length of the anterior aspect of the spinal cord. Another artery called the posterior spinal artery branches off either the posterior inferior cerebellar arteries or the anterior spinal arteries to become the posterior spinal artery. The posterior spinal artery supplies the posterior aspect of the entire length of the cord. The cord also gets its blood supply from what are called radicular arteries. For now we will overlook the possible role of the anterior and posterior spinal arteries in chronic ischemia of the spinal cord and focus on the vertebral-basilar arteries and ischemia of the brain. In brief, chronic ischemia of the cord may play a role in amyotrophic lateral sclerosis and primary lateral sclerosis.
The vertebral-basilar arteries supply most of the the motherboard of the brain, which is the brainstem and cerebellum. Except for the nose and eyes it also supplies all the cranial nerves, which control the muscles and senses of the head and neck down to the shoulders, as well as autonomic function of the internal organs via the vagus cranial nerve. In this regard, the vertebral-basilar arteries also supply the hypothalamus, which is the control center for autonomic vegetative functions in the body, and the thalamus, which is the sensory switchboard or router of the brain.
In additon to the brainstem and cerebellum, the vertebral-basilar arteries supply the inner parts of the temporal, and the inner parts and rear pole of the occipital lobes of the brain. Among other things, the inner temporal lobe is important to memory. The occipital lobe is important for interpreting visual signals which is likewise dependant upon memory.
The areas located at the tail ends of the anterior and posterior blood supply routes are called the watershed areas of the brain. The watershed areas of the brain are the weakest point in the blood supply routes and oftentimes are the ones most affected by decreases in blood flow. Like the brain the cord also has watershed areas which I will leave out of this discussion. One of the watershed areas in the brain is around the periventricular areas where MS lesions are often found. Alzhiemer’s and migraine headaches also have a predilection for periventricular white matter lesions. Many researchers believe that the white matter lesions in MS, migraines and Alzheimer’s disease are caused by chronic ishemia.
While the lesions are typically found higher up in the brain above the covering over the cerebellum, many of the symptoms associated with MS come from cranial nerves supplied by the vertebral-basilar arteries. Symptoms such as dizziness and fatigue are mostly likely signs of ischemia. Likewise, the lesions seen in certain cases of MS, especially those associated with migranous symptoms are most likely caused by chronic ischemia. In addition, the vertebral-basilar arteries are the ones most commonly involved in ministrokes called transient ischemic attacks. The design of the skull, spine and circulatory system of the brain predisposes humans to upper cervical strains and subsequent compression and back pressure against the posterior blood supply routes, which are the vertebral-basilar arteries. The outcome is chronic ischemia in the areas of the brain they supply.
In my next post I will discuss upper cervical strains and deformation of neurovascular tunnels. Upper cervical strains and deformation of critical neurovascular tunnels are most likely one of the major causes of chronic ischemia and edema in the brain. They may also play a role in normal pressure hydrocephalus, but that’s an entirely different story more related to Parkinson’s and Alzheimer’s disease.
For additional information on this and related topics visit my website at http://www.upright-health.com.




dear Dr. Flanagan, what an awesome wealth of information. this post as well as your other ones on the results of upright posture and disease. i really believe now that is the main culprit with having bad posture in the neck area and m.s.for so many years! there are 2 NUCCA doctors in the Cleveland Ohio USA area. so i am going to setup a consultation to see what they think if they could do something for me. are there neck exercises that i could do to strengthen the neck area. I’m sure getting older is not helping as i am 55 years old. this makes so much sense now how venous circulation for the brain is do important! but thank you again for you marvelous insight into this matter of posture and disease. this also explains why ccsvi treatment does not help everyone.
thank you again, dave
Thanks for the compliment Dave. Blood vessels of the brain and cord follow the curves of the spine. Abnormal curvatures of the spine likewise cause curves in the bloodstreams of the brain and cord. Curves in streams and rivers cause turbulant flow and eddies. Some researchers have suggested that turbulant blood and CSF flow may play a part in poor tissue perfusion and MS lesions. Ask your chiropractor about neck exercises after you have been evaluated.
Dear Dr FLanagan,
I recently had a ct scan with the results being, moderate periventricular low attenuation. relating to Chronic Subcortical ischaemia. incidental basal ganglia calcification is also noted. would be very grateful if you could please clarify this for me and also any treatment that i should be looking at. thank you
Hello Anisa, The problem is the “chronic subcortical ischemia.” Do you have any MS signs or symptoms? Do you have migraine headaches? Tell me a little bit more about your case. Why was the MRI done? MFDC
Dr Flanagan – I am interested in your thoughts on how to increase the blood flow through the vertebral veins. I understand that the vertebral veins are too small to be opened with angioplasty so how would you recommend treating reduced blood flow in those vertebral veins. In my case, I have had ultra sound that shows no blockages in the jugular veins but reduced flow in the vertebral veins. I am awaiting venography. Thank you.
One of the best ways to improve blood flow through the vertebral veins is to remove restrictions to flow caused by problems in the cervical spine. The design of the skull and spine predisposes humans to problems in the cervical spine, especially in the upper cervical spine and base of the skull.
Make sure your blockage isn’t due to fibromuscular dysplasia. DONT EVER go to a chiropractor which is very dangerous to people with any type of connective tissue disease. The reduced blood flow could be a result of this misunderstood disease. Ask your General Practitioner to listen to your vascular beds for what’s called a bruit, or a whooshing sound. If he/she hears this, then they should order a non-invasive ultrasound of your vascular beds from your neck to pelvic region.
Thank you for your prompt reply.I had the mri as a result of a fall to the head.however no evidence of any fracture and ventricles appear normal.In regards to headaches i do get headaches regularly i do not think that they are migraine as i do not feel nausea but rather that the pain starts in my back and works it’s way up to my head, resulting in a a stiffen back and neck and a clogged painful feeling in the head and behind the eyes. i am not familiar with ms symptoms or signs.the doctor that i consulted on this suggested that i have blockages to the veins . not sure which veins.what would you suggest please .and What is incidental calcification please
Anisa, I apologize for not getting back sooner. Somehow your message got overlooked. To answer your questions, you most likely hurt your neck when you hit your head in the fall. Since the fall you have been getting headaches and stiff necks along with a clogged painful feeling in the head and behind the eyes. These are signs of a basic neck headache. You aren’t even close to having signs or symptoms of MS. Coincidental calcification is good news as it means nothing. Your MRI is also normal. Get your neck checked.
Dear Dr Flanagan,
Thank you for your advice, certainly a relief to know that it is nothing to worry nabout. i will get my neck check . thanks once again
De Flanagan – Thankfully I am not as seriously debilitated as others who have written you but I am on a quest for prevention given what I believe are some apparent markers in my medical history. I would like your opinion on what I should do given this info.
1. Family history – Dad had Parkinson (but played college football in the 1940’s), Mom had very hi blood pressure, TIA’s, dementia -died at 74.
2. In 04 I complained of neuropathy and ended up being tested for MS – which showed I did have lesions but it was dismissed as being caused by the emergency tracheotomy at age 2 and the lack of oxygen to the brain. My symptoms did not progress and was forgotten.
3. In 06 routine eye exam showed glaucoma signs. Further testing showed some indications but not significant (just like the brain mri tests)
4. Also in about 06 began to have migraines but only about twice a yr.
5. Have always been considered flighty – air-head – etc. Have a real problem with short and long term memory – but am a college grad.
6. Have always had terrible balance – very uncoordinated.
7. And for what it’s worth my firstborn has Asperger’s syndrome.
I am 60 – healthy (low to avg BP)- active and happily married. My biggest fear is Alzheimer’s – have never been to a chiropractor – it just seems there could be a connection to all these granted minor symptoms. Could it all possibly be related to lack of blood flow to the brain?
I would greatly appreciate your thoughts. You’ve been very giving and helpful to others.
Hello John, You have migraines, memory and balance problems which suggest decreased blood supply to the brain. You also have glaucoma which is probably likewise related to decreased blood flow and you have suspicious hyperintensity signals which can also indicate decreased blood flow called ischemia. Lastly, you have low blood pressure which can be a cause of decreased blood flow to the brain.
Because of the migraines and balance problems I would certainly get your upper cervical spine checked and corrected. It will help maximize blood and CSF flow through the upper cervical spine and base of the skull, which will probably help memory as well. Beyond that you need to exercise to get blood flow going and you need a sound diet that supports healthy circulation. You don’t have to be a saint when it comes to diet and exercise but you don’t want to be a sinner either. Moderation is the key.
Great info – I will definitely pursue your recomendations – you did not comment on the brain lesions specifically. Is it possible I’m still a candidate for MS or is it more likely from the tracheotomy?
Dr – the service you provide to those fortunate enough to find your website is beyond measure – we are all grateful!
Thanks for the compliment. The hyperintensity signals are most likely due to decreased blood flow called ischemia. They may well have been caused by whatever provoked the tracheotomy, or it could be indicative of chronic poor blood flow. But the hyperintensity signals don’t correlate with MS in light of your signs and symptoms.
My mother 52 years old and have amyotrophic lateral sclerosis …
Four months ago my mother worked ray Doppler … and we found a narrow and clogged on both sides of the neck … then worked ccvsi
Improved after the operation and continued improvement for about a month .. then stopped .. then began to decline, as is known about the disease …
My question is could be the reason that the improvement is to prevent them from clogging the blood vertebrates .. and that does not work with the expansion ..?
Is the discovery of a narrow possible by MRV OR MRI
Because I have pictures of the neck and head?
And the extent of improvement expected from the expansion? Is conducted befor by or is it just a hypothesis has not been applied yet?
Interesting thoughts…..would it be safe to say that in terms of prodromal symptoms, a persistent:
1. high blood pressure might be suggestive of a venous stenosis type etiology
2. low blood pressure might be suggestive of an ischemic type etiology
Seems you can’t win;) These two seem like they would somehow be related….or have a cause/effect type relationship, over time. Bad habits leading to bad things. Leading to more complicated bad things. ie. low arterial pressures possibly leading to venous collapse/stenosis down the line. Then you’re stuck in a confusing situation, where venous angioplasty may help…as long as you keep the arterial pressure/flow up. The human body…what a thing. Maybe we’ll never truly understand it all.
Dr. Flanagan,
Been having some phosphenes, tingling, issues lately with longstanding fatigue and a remote (2 years ago) history of twisting injury to lower cervical spine. Went to see a NUCCA doc recently, felt sorta strange after he adjusted me from the left side, and this made some of my symptoms worse (tingling isn’t so bad, thought it was down before he adjusted me) along with some confusion, occasional numbness down my left side, and right sided lower neck ache with these findings on CT angiogram (MR pending):
Bodies of lateral ventricles slightly prominent. No evidence of dilatation of temporal horns or of the third ventricle. Otherwise no abnormalities.
Vasculature: at the level of C6, irregularity of the right vertebral artery, which narrows as it abuts the c6 anterior tubercle before entering into the foramen transversarium; however, it resumes a normal caliber distally. No intraluminal thrombus or dissection flap. Could be a normal anatomic variant, but a focal dissection cannot be excluded given the unusual vessel contour. No other vascular abnormality identified.
I’ve always had low blood pressure and slept on my stomach with my head twisted to the left. Would this seem like an ischemic presentation for my symptoms? I realize there is no vein imaging here. There’s also the potential for vertebral artery dissection as they say. Needless to say, following this scenario closely, I was more questioning the findings in light of my pre-adjustment symptoms.
Thanks!
MRI normal, ventricles non dilated.
I’m wondering if i’m having longstanding right vertebral artery flow impediment, which have slowly begun to give me ms type symptoms…possibly exacerbated by the adjustement, stretching the artery a bit/compressing it against the vertebrae?
Never had a major problem with fatigue during exercise, but before and after was pretty tired.
Hello Frank, It does sound as though some of your symptoms can be related to vertebral-basilar artery ischemia. The twisting injury to your lower neck two years ago could certainly be contributing to the problem. NUCCA is extremely gentle and unlikely to cause any harm to the arteries. In fact it should improve blood flow. On the other hand, it can cause musculoskeletal stress as the head and neck adjust to changes and shifts in position. In any case you need to let the doctor know so he can monitor your condition and make adjustments to his procedure if necessary.
Hello Dr. Flanagan,
Kind of curious as to where the slight prominence of the lateral ventricles would fit in with all of this. Also, if you were to increase blood inflow through the vertebral arteries given the imaging, might it not make the ventricles enlarge down the road?
Hello Nirav, A slight prominence of the lateral ventricles suggests possible increased CSF pressure inside the ventricles. In answer to your second question, blood flow in the brain is closely controlled by the autonomic nervous system and remains fairly stable. In other words, for the most part, you can’t increase blood flow to the brain. Conversely, you can cut the flow down by compressing arterial pathways. Lastly, CSF production is not determined by arterial blood flow.
I have been diagnoised with ismich disease, h polari, diabetic just resently and I spend a lot of time in the E. R. I found your artical helpful. Thank you. Is there a relationship between the 3 diseases? The doctors told me that I had high blood sugar but now its low blood sugar resently. The clinic I am trying to move away from act like oh you’ll be okay. Like they aren’t concerned. Would you please draft a little more on this topic. Thak You.
Hello Michael,
I presume you are referring to ischemic disease, Helicobacter pylori and diabetes (high blood sugar). In this regard, your problems most certainly may be connected. You have problems with digestion that starts in the stomach. Weak stomach acid can cause chronic anemia, which can further lead to chronic inflammation. The bacteria in the stomach also suggests possible chronic inflammation and diabetes is also associated with chronic inflammation, as well as vascular degeneration and poor blood flow. Chronic inflammation can cause chronic low grade anemia. Chronic anemia and decreased blood flow due to degenerated blood vessels can lead to chronic ischemia.
Please help had an MRI scan and they said that Ive got tiny focalhigh signal intensities are seen in the left side of the phone and the left middle cerebellar peduncle on axial flair images 6 and 7 these are non- specific and may represent focal chronic ischaemic lesions thanks am worrying don’t unerstand
Hello Yvonne,
I think that you are referring to the pons when you mention the left side of the “phone.” The pons is the middle part of the brainstem that sits between the midbrain and medulla. The cerebellum or hindbrain, is also part of the brainstem located behind the pons. You further mention that you have 6 or 7 non specific lesions in the left middle cerebellar peduncle. The peduncles are communication links that connect the cerebellum to the brainstem. The brainstem and cerebellum get their blood supply from the vertebral arteries that pass through the cervical spine. I suspect you may have migraines. The white spots are most likely signs of chronic ischemia in the distribution of the left vertebralbasilar artery.
Condensed version: Hx fibromyalgia, chronic headaches, migraines, neck stiffness, hypokalemia. For past year and a half: ridiculous fatigue, leg weakness, legs feel like lead, facial numbness,muscles spasms, increase of non-migraine auras, eye twitches for weeks on end, etc. ANA speckled 1:80. Primary suspected MS; sent to neuro. Brain MR w/wo & Cervical MR w/o. Report states: bilat small scattered nonenhancing supratentorial periventricular to deep white matter T2 intense foci. mild chronic microvascular cerebral ischemia”. My neuro has interpreted that report as arteriosclerosis. (I’m 42). Couldn’t the ischemia be from past migraines & headaches? or MS? I might add that the brain MRI & cervical MRI were not done with an MS protocol. I’m at a loss here with the neuro not investigating further into my symptoms.
Hello B,
The location of the supratentorial periventricular lesions could be signs of MS demyelination or ischemia. Your history of migraines, severe fatigue, facial numbness, auras and eye twitches make me suspect ischemia. You probably have venous hypertension in the cavernous sinus that is affecting blood flow to the brain and eyes, as well as irritating the occulomotor and trigeminal nerves. The muscles spasms, leg weakness and heaviness could be neurological but they are more likely due to structural issues, especially in the cervical spine.
With all my symptoms, wouldn’t it seem that the neuro should investigate further instead of going with ischemia since I’m only 42? A spinal can be positive without lesions on MR & I’ve yet to be tested for Lyme. Thoughts?
Speaking for myself, I would certainly investigate further. In light of the classic location of your lesions, Lyme disease doesn’t seem likely to me but it’s a good idea to check. I suspect, however, that the ischemia may be due to structural issues not Lyme disease or vascular degeneration. You need a good physcial exam to investigate potential structural issues that can cause ischemia, especially the upper cervical spine. An ultrasound exam of your carotid and vertebral arteries would be helpful.